What is the impact of menopause on estrogen and how does this affect the microbiome?
This Menopause Awareness Month we welcomed a specialist panel to share their knowledge on the link between menopause and the uro-vaginal microbiome. This is such an important topic and we want to keep the conversation going and promote more education and innovation in this area. Today we cover vaginal health, the impact of menopause on estrogen levels and what happens to the microbiome during menopause, hearing from;
Dr Nitu Bajekal, Gynaecologist, and Author of Finding Me In Menopause
Melissa Kramer, Patient Advocate and CEO of Live UTI Free
Chanelle Ryan, Senior Scientist at P.Happi
Dr Ishani Rao, NHS GP, BSc Women's Health, Plant Based Health Professional
Lauren Chiren, Menopause Coach and CEO of Women of a Certain Stage.
What is the vaginal microbiome, and what role does it play in postmenopausal vaginal health?
Dr Nitu Bajekal, Gynaecologist
The vaginal microbiome is quite distinct from other parts of the human microbiome such as the gut microbiome. Unique conditions of the vagina, a muscular tube that connects the neck of the womb to the exterior, ensures it is colonised by a few microbial species, usually lactobacilli and some others. These species can use glycogen, which in turn is under the control of estrogens, producing lactic acid, hence the acidic nature of the vaginal environment and are responsible for acidifying vaginal milieu, helping withstand vaginal infections. However, the composition of the vaginal microbes is only part of the story in maintaining a healthy vaginal environment and is dependent on several other factors, age and physiological status of the vagina, with genetics and ethnicity also possibly playing a role.
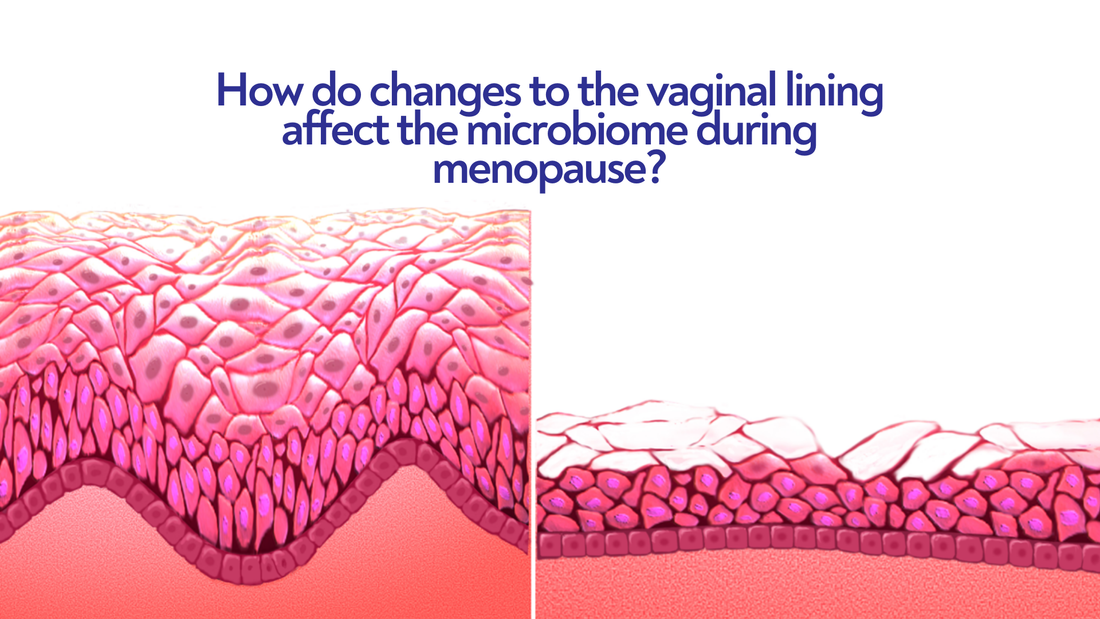
As women get closer to menopause, their levels of estrogen decrease, which causes important changes in the vaginal area. Estrogen helps keep the vaginal walls thick, flexible, and healthy. It also helps produce glycogen, a type of sugar that supports the growth of healthy bacteria in the vagina, specifically Lactobacillus. These bacteria are important because they keep the vagina slightly acidic, which helps prevent harmful bacteria from growing. After menopause, when estrogen levels drop, less glycogen is produced. This leads to fewer Lactobacillus bacteria, making the vaginal environment less acidic. Without enough acidity, harmful bacteria are more likely to grow, increasing the risk of infections like bacterial vaginosis (BV) and urinary tract infections (UTIs).
How does the uro-vaginal microbiome change during menopause? How do these shifts affect symptoms like dryness or infections? What are common experiences from your women in your network?
Melissa Kramer, CEO Live UTI Free
We hear many experiences of frequent UTIs developing during perimenopause. These UTIs often occur alongside vaginal dryness and discomfort during sex. The vaginal and urinary microbiomes are interconnected, so it's not surprising these symptoms can arise in parallel. But why does this happen? The decrease in levels of estrogen during perimenopause leads to a reduction of the 'good' bacteria in the vagina - specifically, Lactobacillus. Lactobacilli are likely protective against UTI, and when there are fewer around, pathogenic bacteria have more opportunity to cause infection. The good news is, we hear from many women who have overcome this problem, with the right treatment.
Chanelle Ryan, Senior Scientist P.Happi®
The vagina has its own unique microbiota. Here, however, low diversity is best. The ideal vaginal microbiota is composed primarily of lactobacilli, with Lactobacillus crispatus being the bacterium most associated with health. The urinary tract is similar, having low diversity and lower amounts of bacteria compared to other body sites, like the gut. It was previously believed that healthy urine was sterile, but as sequencing technology has improved, scientists have discovered a range of organisms that are present even in healthy individuals. In menopause, microbial diversity and abundance further decline as estrogen levels drop, leading to thinner, drier vaginal tissue. This reduction in Lactobacillus populations, a Lactobacillus-depleted or weakened microbiome increases the risk of infections and unwanted symptoms.

Image credit - BruceBlause for Blausen Medical
How do hormonal changes during menopause impact the balance of the vaginal microbiome, and what lifestyle or dietary adjustments can support its health?
Dr Ishani Rao, NHS GP, BSc Women's Health, Plant Based Health Professional
We have been able to visualise changes in the vaginal microbiome that occur as women go through menopause using molecular markers. We can see that reductions in estrogen, and hormonal changes can lead to variation in the levels of ‘good’ bacteria such as Lactobacillus. These healthy bacteria usually exist in a balance in pre-menopausal women, however dysregulation can lead to issues such as thrush, vaginal dryness, skin atrophy and vaginal discomfort. Hormone replacement therapy and vaginal supplements are effective ways of artificially restoring this balance to alleviate symptoms of menopause.
Something that I always choose to discuss with my patients who present with perimenopausal or menopausal symptoms is the benefit of lifestyle modifications on caring for our microbiome (including gut, skin and vaginal). Many patients are familiar with the importance of the gut microbiome, but are not aware that a similar network exists in the vagina. Strengthening our immune system through a healthy diet is a brilliant way to ensure that we are naturally supporting our microbiome to defend against the negative implications of ageing. Ensuring that our meals are filled with colourful whole foods, limiting processed junk foods and cutting out inflammatory ingredients such as animal products is an easy way to improve our entire microbiome.
This is something that I always suggest, either in conjunction with or as a preliminary step to medication- as there are no side effects from consuming a healthy diet!
Lauren Chiren, Menopause Coach and CEO of Women of a Certain Stage
During menopause, hormonal changes - particularly estrogen changes and reduction - can affect the balance of the vaginal microbiome.
Estrogen plays a crucial role in maintaining the health of the vaginal ecosystem, especially by supporting the growth of lactobacilli, beneficial bacteria that help maintain the correct pH level. This acidity protects against harmful bacteria, fungi, and infections. As estrogen levels drop, the environment of the vagina becomes less acidic, reducing the number of lactobacilli and allowing potentially harmful microbes to thrive.
This imbalance can lead to symptoms like vaginal dryness, irritation, itching, infections (such as bacterial vaginosis or yeast infections), and discomfort during intercourse.
Impact of Menopause on Vaginal Microbiome:
- Reduced Lactobacilli: With lower estrogen, lactobacilli decline, leading to less protection from infections
- Increased pH: A less acidic environment fosters the growth of pathogenic bacteria and fungi
- Vaginal Dryness: This can increase the risk of microtears and infections
- Increased Susceptibility to Infections: Women may experience recurrent urinary tract infections (UTIs) and vaginal infections
Lifestyle and Dietary Adjustments to Support Vaginal Microbiome Health:
- Hydration: Adequate water intake supports overall body hydration, which can help alleviate vaginal dryness.
- Probiotics: Consuming probiotic-rich foods like yogurt, kefir, and fermented vegetables or taking probiotic supplements (especially those containing strains of Lactobacillus) may help restore balance to the vaginal microbiome by increasing beneficial bacteria. Always seek advice from a suitably qualified nutritionist or dietitian
- Phytestrogens: These plant-based compounds are said to mimic the effects of estrogen - at very low levels - in the body and may possibly help maintain vaginal health. Foods rich in phytestrogens include flaxseeds, soy, tofu, and whole grains.
- Vaginal Moisturizers and Lubricants: Using correctly pH balanced lubricants, during intercourse and vaginal moisturizers regularly can alleviate dryness and reduce the risk of irritation or microtears.
- Avoid Harsh Soaps and Irritants: Using fragrance-free, gentle cleansers on the genital area helps maintain the natural balance. Avoiding douching is particularly important, as it can disrupt the vaginal flora.
- Healthy Fats: Omega-3 fatty acids, found in fatty fish (salmon, mackerel), flaxseeds, and walnuts, can support mucous membrane health, which includes the vaginal lining.
- Diet Rich in Fibre: A high-fibre diet can support digestive health, and a healthy gut microbiome is linked to a balanced vaginal microbiome. Whole grains, fruits, and vegetables are key.
- Limit Sugar, Alcohol and Processed Foods: A high-sugar diet can encourage the growth of yeast, potentially leading to imbalances and infections. Reducing sugar intake can support a healthier vaginal environment.
Thank you to our panel for sharing their knowledge and insights with us. Do you have questions you’d like us to answer next? Let us know below.